PLGA: A Versatile Copolymer for Nanoparticle Design & Development
Poly (lactic-co-glycolic acid) or PLGA has been a widely studied polymer in the pharmaceutical industry because of its compatibility and safety.1 PLGA with its unique LA/GA composition ratios and molecular weight, provides a viable barrier to protect the premature release and degradation of drugs encapsulated in microspheres or nanoparticles. Because of its biocompatibility and biodegradability in nature, it has been used in several oncology and lifesaving drugs.2
To optimize PLGA in drug development, teams must understand its chemistry, properties, applications, and regulatory aspects. Ascendia Pharmaceutical Solutions’ scientists are well-versed in these aspects. They also have their proverbial fingers on the pulse of the future trends in the industry, especially those requiring the development of long-acting injectables (LAIs) to treat rare diseases and for life cycle management. These traits are reasons we are the CDMO Partner of Choice for a growing number of pharmaceutical companies.
PLGA Structure
Depending upon the molar ratios of lactic acid and glycolic acid used in the synthesis, PLGAs used for pharmaceutical applications are composed of 75% lactic acid and 25% glycolic acid and/or 50% each of lactic acid and glycolic acid. PLGA (Tg 40°C-60°C) is typically soluble in a wide range of chlorinated solvents like methylene chloride, chloroform, and hexafluoro isopropanol (HFIP) and non-chlorinated solvents, such as THF, acetone, DMSO, glycofural, ethyl acetate, ethanol, N-methyl pyrrolidone, methyl ethyl ketone, acetonitrile, isosorbid dimethyl ether, dioxane, among others.3
In water, PLGA biodegrades by hydrolysis of its ester linkages. The methyl side group in poly lactic acid moiety makes it relatively more hydrophobic than polyglycolic acid; hence, lactide-rich PLGA copolymers are less hydrophilic and susceptible to degradation by hydrolysis.4 The higher the lactic acid, the slower the degradation and vice versa. In LA/GA 1:1 copolymer, the degradation is fast, leading to formation of lactic acid and glycolic acid within three months.
Lactic acid is metabolized in tricarboxylic acid cycle and gets excreted via carbon dioxide and water, whereas, glycolic acid metabolizes the same pathway as lactic acid, and is excreted through the kidneys. Glycolic acid is also metabolized into oxalic acid, which may lead to systemic toxicity in the body during implantation or longer circulation of PLGA microspheres.
Characteristics and Drug Delivery of PLGA Microspheres
The challenges in utilizing PLGA stems from encapsulating hydrophilic drugs into hydrophobic PLGA. Leaping the hurdles associated with reducing burst release and increasing encapsulation efficiency of hydrophilic drugs in PLGA require additional functional hydrophilic layers. Additional functional layers, such as hydrophilic gels/hydrogels around the PLGA core-shell microspheres for sustained release, are used.
.jpg?width=524&height=347&name=plga%20fig%201%20(002).jpg) PLGA microsphere’s core shells are distinct. Depending on the usage of nanoparticles, they may have varying core shapes, internal structures, shell thicknesses, and morphologies and porosities.5 The latter is most explored for designing and increasing drug loading in PLGA microspheres for controlling the delivery by changing the porosity of the PLGA cores. Pore size and porosity of PLGA microspheres with broader surface area and lower density play an important role in faster releasing of drugs.6
PLGA microsphere’s core shells are distinct. Depending on the usage of nanoparticles, they may have varying core shapes, internal structures, shell thicknesses, and morphologies and porosities.5 The latter is most explored for designing and increasing drug loading in PLGA microspheres for controlling the delivery by changing the porosity of the PLGA cores. Pore size and porosity of PLGA microspheres with broader surface area and lower density play an important role in faster releasing of drugs.6
A number of porogen agents such as sodium chloride, ammonium bicarbonate, a tri-block copolymer Poloxamer 407, sodium oleate, gelatin, bovine serum albumin, cyclodextrins, and mineral oils, have been investigated for creating porous PLGA microspheres. Porosity can be modified by solvents and polymer concentrations.
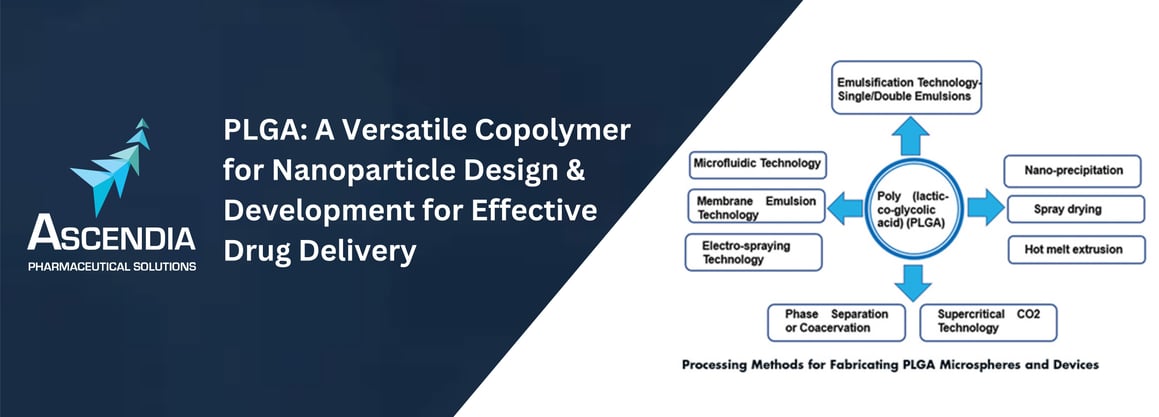
Preparation of PLGA Microspheres and Devices
Emulsion and double emulsion solvent evaporation process – (W/O/W) – is simple. It requires the drug to dissolve in an aqueous solution (W) with or without excipients, and the PLGA is dissolved in organic solvents, preferably in methylene chloride or ethyl acetate (O). O/W emulsions are formed by adding and mixing of an aqueous solution of drug in PLGA dissolved in organic solvent. The first emulsions (O/W) are then mixed with a second continuous aqueous solution containing a surfactant, such as polyvinyl alcohol (PVA), to yield W/O/W emulsions. Removal of an organic solvent through diffusion or extraction or evaporation leads to solidification of the PLGA microspheres.
Ascendia Pharmaceutical Solutions is adept at multiple approaches to address PLGA, including:
- Phase Separation or Coacervation – Emulsions are prepared by addiing aqueous drugs into PLGAs dissolved in methylene chloride. A coacervation agent, such as silicon oil, is gradually added into primary emulsions to promote phase separation. As methylene chloride is extracted into the silicon oil, PLGA microspheres get precipitated, which are further hardened by washing with apolar solvents, such as heptane or hexane.
- Spray Drying – This atomization-based process requires the spray drying of O/W emulsions prepared by aqueous drug mixing with PLGA dissolved in methylene chloride. The resulting spray dried powder of PLGA microspheres entrapped with the drug are dried to remove the residual solvents.
- Hot Melt Extrusion (HME) – Hot melt extrusion is an ideal solvent-free method for creating implants by processing a PLGA at temperatures higher than glass transition temperature (Tg) of polymers, PLGA/PLA. The resulting extrudates or rods can be used as implants.
- Nano-precipitation – This process requires dissolving the drug and PLGA in water-miscible organic solvents and injecting into an aqueous-phase water. The result is a solvent exchange by diffusion and nanoprecipitation of drug into PLGA depots, ideally suited as reservoirs for in situ delivery.
- Supercritical CO2 – It involves the injection of drug dissolved in methanol into SC-CO2 as an anti-solvent, which acts as an extractant for methanol, and instantaneously leads to precipitation of drug nanoparticles, which is encapsulated in PLGA with well-dispersed drug in microspheres.
- Electro-spraying – It is based on atomization of drug and PLGA in an organic solvent, which is subjected to electric voltage to produce the particles. It is commonly used in preparation of solid dispersions of poorly soluble drugs.
- Microfluidics Technology – It offers better control over particle size distribution and is amenable to low volumes. Microfluidic systems fitted with 1-mm channels have shown to be suitable for large-scale production of PLGA nanoparticles.
- Membrane Emulsification – A relatively new technology that combines emulsification methods and porous membranes. The dispersed phase is pressed through a membrane and the droplets formed are carried away with the continuous phase. The result is a more uniform and controlled particle size with narrow distribution and high drug encapsulation efficiency compared to emulsification solvent evaporation technology.
PLGA Nanoparticles in Drug Delivery of Blood Brain Barriers
The blood brain barrier (BBB) protects the central nervous systems (CNS) from unnecessary entry of unwanted substances, posing challenges in delivery of molecules for treatment of glioblastoma and other brain diseases. These tight junctions (TJs) formed by a complex network of proteins and linked with the cytoskeleton can restrict the passage of substances from the bloodstream to the brain. Many therapeutic agents can’t overcome the BBB. PLGA nanoparticles (hydrophobic in nature) can penetrate the BBB and can be used as carries for delivery of drugs.7 PLGA NPs with surface-modified surfactants also improved the cellular uptake by permeation of BBB.
.jpg?width=2182&height=728&name=PLGA%20table%201%20(002).jpg)
Table 1 (above) lists the brain uptake of surface-modified PLGA nanoparticles in animal models.7 It is evident that carotid administration showed relatively higher brain uptake than intravenous route of administration.
PLGA Nanoparticle Formulation Capabilities
Our in-house capabilities in upstream and downstream cGMP manufacturing of injectable lipid-based LipidSol® and polymeric-based PLGA NanoSol® have been well utilized within our state-of-the art sterile facility with ISO-certified cleanrooms. Table 2 (below) shows the preparation of carvedilol-loaded PLGA nanoparticles from PLGA (50:50 LA/GA).8
.jpg?width=2168&height=356&name=PLGA%20table%202%20(002).jpg)
The method for preparation of carvedilol-encapsulated PLGA nanoparticles involves dissolving the drug and polymer (1:10) in methylene chloride by thorough mixing as an oil phase. An aqueous solution containing 2% polyvinyl alcohol (PVA) with MW 9,000-10,000 D was used as a surfactant. API/polymer oil phase was added slowly in a PVA aqueous solution dropwise and mixed thoroughly, keeping the oil/water phase ratio 1:7. The entire solution was mixed thoroughly in ice cold water to emulsify by sonication - to achieve the desired particle size.
The resulting nanoparticles were poured and mixed in 2% PVA aqueous solution for three hours and collected following the centrifugation for 30 minutes at 14,000 xg. The drug/PLGA nanoparticles were collected by discarding the supernatant and washed repeatedly with water. The resulting pure concentrated drug/PLGA nanoparticle suspension once again was passed through filter -, and centrifuged again for 10 minutes at 14,000 xg to remove any free drug. It was lyophilized with sucrose (10%-30%) as cryo-protectant or used freshly or stored at 4°C for weeks. Drug loading was determined by HPLC, and release profile of the drug was assessed.
Summary
Designing PLGA micro/nanospheres requires careful selection of the fabricating process. For example, membrane emulsion and microfluidics methods yield PLGA microspheres with higher drug encapsulation efficiency and with lower polydispersity index, i.e., PDI of 0.048 with carvedilol encapsulated PLGA.8
Taken collectively, Ascendia Pharmaceutical Solutions’ capabilities in the downstream and upstream manufacturing process can lead to development of PLGA-based nanoparticle-encapsulated drugs for life-threatening ailments. State-of-the-art cGMP manufacturing suites designed to handle organic solvents, including methylene chloride, are in place for future generations of polymeric and lipid-based nanoparticles for unmet medical needs.
Contact us to learn how we can be your Partner of Choice for your PLGA projects.
References
- X. Shen, T. Li, X. Xie, Z. Chen, H. Yang, C. Wu, S. Deng and Y. Liu, PLGA based drug delivery systems for remotely triggered cancer therapeutic and diagnostic applications, Frontiers Bioeng. Biotech., 2020, 8, 381. doi:10.3389/fbioe.2020.00381.
- M. Alvi, A. Yaqoob, K. Rahman, S. M. Shoaib and M. S. H. Akash, PLGA based nanoparticles for the treatment of cancers: current strategies and perspectives, AAPS Open, 2022, 8, 12;https://doi.org/10.1186/s41120-022-00060-7.
- E. Lagreca, V. Onesto, C. D. Natale1, S. L. Manna, P. A. Netti and R. Vecchione, Recent advances in the formulation of PLGA microparticles for controlled drug delivery, Prog. Biomaterials, 2020, 9, 153-174.
- H. K. Makadia and S. J. Siegel, Poly Lactic-co-Glycolic Acid (PLGA) as Biodegradable Controlled Drug Delivery Carrier, Polymers, Polymers, 2011, 3, 1377–1397. doi:10.3390/polym3031377.
- J. Lee, Y. J. Oh, S. K. Lee, and K. Y. Lee, Facile control of porous structures of polymer microspheres using an osmotic age pulmonary delivery. J Control Release, 2010, 146, 61–67.
- C. Busatto, J. Pesoa, I. Helbling, J. Luna, and D. Estenoz (2018) Effect of particle size, polydispersity and polymer degradation on progesterone release from PLGA microparticles: experiment and mathematical modeling. Int. J. Pharm. 2018, 536, 360–369.
- J. Li and C. Sabliov, PLA/PLGA nanoparticles for delivery of drugs across the blood-brain barrier, Nanotechnol Rev. 2013, 2, 241–257; DOI 10.1515/ntrev-2012-0084.
- V. Ivanova, K. Maeda, W. Wang, D. Guo and J. Huang, Parenteral sustained release delivery of carvedilol disperse systems, US Patent, 10,792,244 (October 6, 2020).